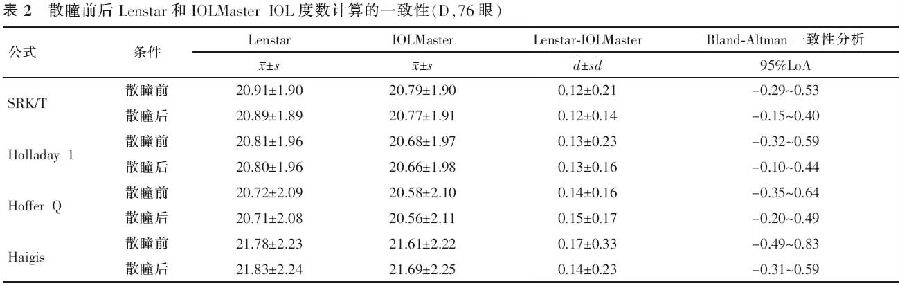
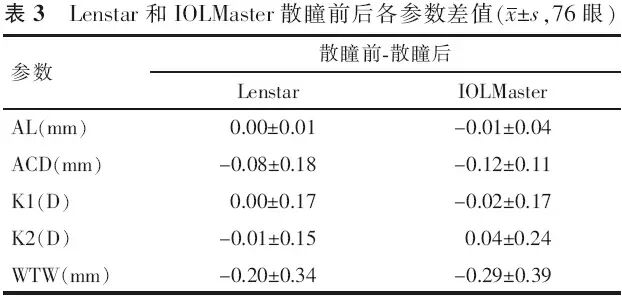
【摘要】 目的 评估新型光学生物测量仪Lenstar测量白内障患者眼球生物结构参数和IOL度数计算的准确性,并研究散瞳对其测量结果的影响。方法 前瞻性临床研究。应用Lenstar和IOLMaster分别对76例(76眼)年龄相关性白内障患者散瞳前后的眼轴长度(AL)、角膜曲率(K1和K2)、前房深度(ACD)及白到白距离(WTW)进行测量,并利用SRK-T、Hollday 1、Hoffer Q和Haigis 4种公式计算IOL度数。同一医生完成所有的测量,2个仪器测量顺序随机。散瞳前2个仪器的测量结果的差异性和一致性及散瞳后2个仪器的测量结果的差异性和一致性分别做配对t检验和Bland-Altman分析;对散瞳前后2个仪器测量结果及IOL度数的比较采用Pearson相关分析和配对t检验。结果 Lenstar和IOLMaster散瞳前后测量的AL、K1、K2均高度相关(r均>0.90)。2种仪器散瞳后测量的ACD和WTW值[Lenstar:(3.13±0.34)mm和(11.76±0.51)mm;IOLMaster:(3.15±0.34)mm和(12.15±0.47)mm]均大于散瞳前[Lenstar:(3.05±0.35)mm和(11.56±0.55)mm;IOLMaster:(3.03±0.34)mm和(11.85±0.44)mm],且差异具有统计学意义(t=-3.98、-5.09、-9.00、-6.52,P<0.01)。2种方法测量的WTW的95%LoA散瞳前为-1.20~0.61 mm,散瞳后为-1.09~0.33 mm,一致性较差,其余参数一致性较好。散瞳后Haigis公式依据IOLMaster测量结果计算的IOL度数比散瞳前大(0.08±0.29)D,差异有统计学意义(t=-2.31,P<0.05)。结论 Lenstar是一种精确性高的眼球生物参数测量和IOL度数计算工具,可替代IOLMaster行白内障术前检查。散瞳影响ACD和WTW的测量,但对IOL度数的计算影响很小。
【关键词】 Lenstar; IOLMaster; 散瞳; 生物结构测量; 白内障; 人工晶状体度数计算
DOI:10.3760/cma.j.issn.1674-845X.2014.05.010
基金项目:浙江药卫生科技计划项目(2012KYB135);浙江省教育厅科研项目(Y201223147);温州市科技局资助项目(Y20110045,Y20120176)
作者单位:325027 温州眼科和视光仪器评估与应用研究所温州眼视光学院
通信作者:赵云娥,Email:zye@mail.eye.ac.cn
Effect of cycloplegia on ocular parameters and intraocular lens calculation with Lenstar on patients with cataracts
Lin Huayou, Huang Jinhai, Li Yuanguang, Su binbin, Wu Ge, Gong Xianhui, Cai Junyong, Zhao Yun′e. School of Optometry and Ophthalmology, Eye Hospital of Wenzhou Medical University, Wenzhou 325027, China
Corresponding author:Zhao Yun′e,Email:zye@mail.eye.ac.cn
【Abstract】 Objective To evaluate ocular biometry measurements and intraocular lens (IOL) power calculation with the new optical biometry Lenstar, and to review the effect of cycloplegia on biometric parameters and IOL power calculation on patients with cataracts. Methods In this prospective, comparative, observational study of ocular measurements on 76 cataracts, measurements of axial length (AL), corneal curvature (K1, K2), anterior chamber depth (ACD) and white to white (WTW) were performed by a single operator using the Lenstar and the IOLMaster before and after pupil dilation. The sequence of the measurements pre- and post-cycloplegia between the two devices was randomized. Pre- and post-cycloplegic IOL power were performed with 4 formulas (Sanders-Retzlaff-Kraff/Thoretical, Holloday 1, Hoffer Q and Haigis) using an A constant of 118.0. The refractive target was post-operative emmetropia. Bland-Altman plots were applied to evaluate the agreement and differences between the two devices. The differences between pre- and post-cycloplegic measurements as well as IOL power calculations with the 2 devices were assessed using a paired t test, and their correlation was reviewed by the Pearson coefficient. Results The pre- and post-cycloplegic measurements of AL and K1 and K2 performed with both devices correlated well (Lenstar, r=1.00, 0.990, 1.00, respectively) and (IOLMaster, r=1.00, 0.99, 0.99, respectively). ACD and WTW were significantly longer after pupil dilation: Lenstar (3.05±0.35 mm, pre-cycloplegia) vs (3.13±0.34 mm, post-cycloplegia) with ACD (t=-3.98, P<0.01) and (11.56±0.55 mm, pre-cycloplegia) vs (11.76±0.51 mm, post-cycloplegia) with VCD (t=-5.09, P<0.01); IOLMaster,(3.03±0.34 mm, pre-cycloplegia) vs (3.15±0.34 mm, post-cycloplegia) with ACD (t=-9.00, P<0.01) and (11.85±0.44 mm, pre-cycloplegia) vs (12.15±0.47 mm, post-cycloplegia) with WTW (t=-6.52, P<0.01). All measurements except WTW were closely related. The 95%LoAs in both devices were -1.20~0.61 mm pre-cycloplegia and -1.09~0.33 mm post-cycloplegia. The differences between pre- and post-cycloplegic IOL power were not statistically significant except for the IOLMaster using the Haigis formula (t=2.31, P<0.05), but the values were not clinically different. Conclusion Lenstar biometry provides precise measurements and correlates well with IOLMaster, thus either can be used for the preoperative examination of cataracts.
【Key words】 Lenstar; IOLMaster; Cycloplegia; Biometry; Cataract; Intraocular lens power calculation